What Is Plantar Fasciitis?
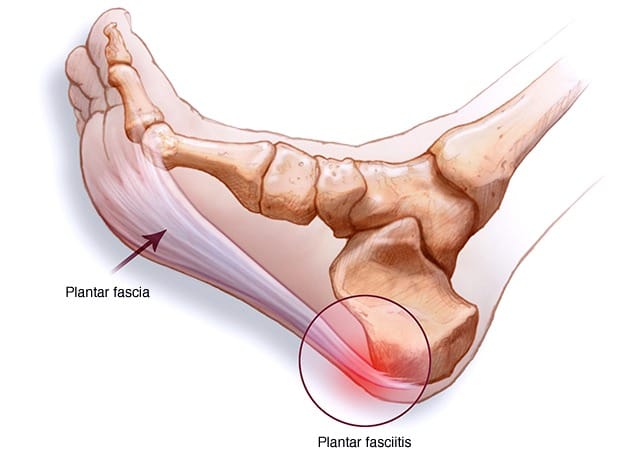
Plantar fasciitis is a common foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot.
Plantar fasciitis is a term that might not be familiar to everyone, but for those who have experienced it, the condition is synonymous with persistent heel pain. It is an inflammation of the plantar fascia, a thick band of tissue that runs from the heel bone to the toes.
Key Takeaways:
- Plantar fasciitis is a common condition causing heel pain due to inflammation of the plantar fascia.
- Risk factors include obesity, certain exercises, foot mechanics, and occupations requiring long periods of standing.
- Treatment options range from home remedies and physical therapy to medical interventions in severe cases.
Plantar fasciitis is a term that might not be familiar to everyone, but for those who have experienced it, the condition is synonymous with persistent heel pain.
It's a common foot ailment that can affect your daily activities and quality of life. In this comprehensive guide, we'll explore what plantar fasciitis is, its causes, symptoms, and the various treatment options available.
Understanding the Plantar Fascia
The plantar fascia is a thick band of tissue that runs across the bottom of your foot, connecting the heel bone to the toes. It supports the arch of your foot and absorbs shocks when you walk. When this tissue becomes inflamed, the condition is known as plantar fasciitis.
This inflammation can cause a stabbing pain that usually occurs with your first steps in the morning.
As you get up and move more, the pain typically decreases, but it might return after long-standing or standing after sitting.
Anatomy of a Foot
The human foot is a marvel of biomechanical engineering, comprising intricate structures that facilitate movement, support body weight, and absorb shock. Understanding the anatomy of the foot is essential for athletes, healthcare professionals, and anyone interested in foot health.
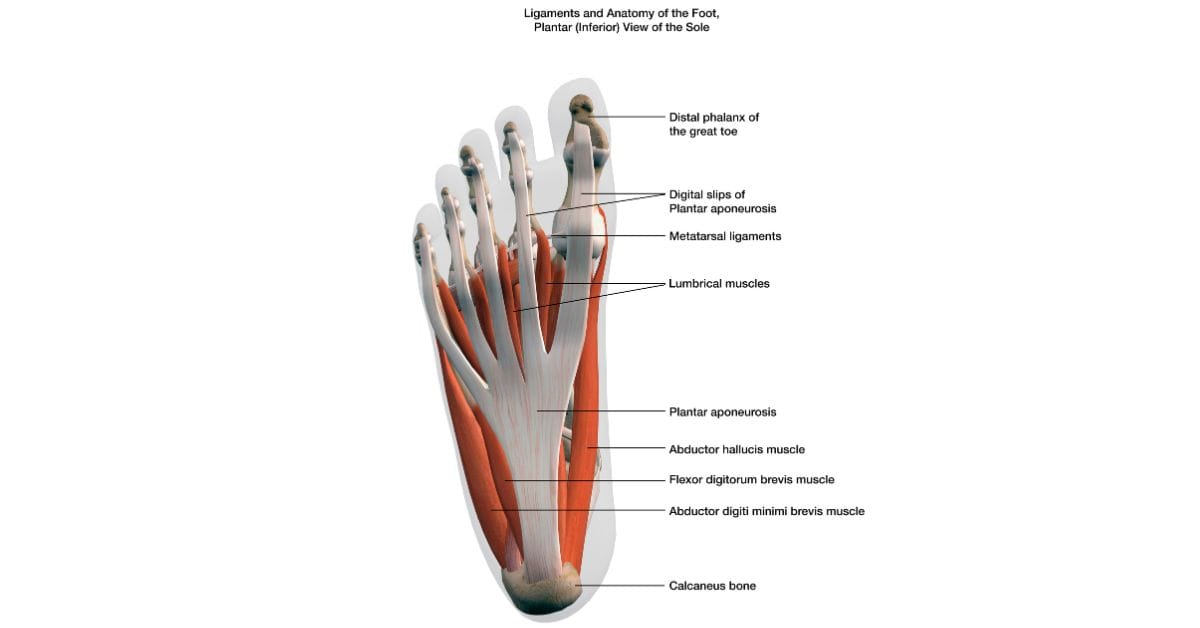
In this article, we'll delve into the fascinating world of foot anatomy, exploring its bones, muscles, ligaments, and functions, to gain a deeper appreciation for this vital part of the human body.
Causes and Risk Factors
Several factors can contribute to the development of plantar fasciitis. One of the primary causes is excessive strain on the plantar fascia, often due to overuse or repetitive stress.
This can happen to runners, dancers, or anyone whose activities place a lot of pressure on the heel and attached tissue.
Additionally, people who are overweight and those who wear shoes with inadequate support are at higher risk.
Certain foot mechanics, like having a high arch or flat feet, can also contribute to the distribution of pressure on the plantar fascia, leading to the condition.
Symptoms
The most telling symptom of plantar fasciitis is a sharp pain in the heel, particularly with the first steps after waking up or after a long period of rest.
The pain can also flare up after prolonged activity but not usually during it. Some people describe the pain as a dull ache or a burning sensation on the bottom of the foot extending outward from the heel.
If you're experiencing consistent heel pain, it's crucial to consult a healthcare professional for an accurate diagnosis, as these symptoms can also indicate other conditions.
Diagnosis
To diagnose plantar fasciitis, a doctor will typically perform a physical exam to check for tenderness in your foot and the exact location of the pain.
This ensures that the pain is not the result of a different foot problem. An X-ray or MRI might be ordered to rule out issues like a bone fracture or pinched nerve.
While imaging tests cannot diagnose plantar fasciitis, they can detect other problems that could be causing the pain.
Home Remedies and Self-Care
For many people with plantar fasciitis, home remedies can provide significant relief.
Resting, icing the affected area, and over-the-counter pain relievers can help reduce inflammation and alleviate pain.
Stretching exercises for the Achilles tendon and plantar fascia can also be beneficial.
Additionally, wearing supportive shoes and avoiding barefoot on hard surfaces can prevent further strain on the plantar fascia.
Physical Therapy and Exercises
Physical therapy can be an effective treatment for plantar fasciitis. A physical therapist can show you a series of exercises to stretch the plantar fascia and Achilles tendon and to strengthen lower leg muscles, which stabilize your ankle and heel.
Another part of physical therapy may include applying athletic taping to support the bottom of your foot.
Medical Treatments
If home remedies and physical therapy aren't enough, medical treatments may be necessary.
These can include corticosteroid injections to reduce inflammation, extracorporeal shock wave therapy to stimulate healing, and in rare cases, surgery to detach the plantar fascia from the heel bone.
It's essential to discuss these options with a healthcare provider to determine the best course of action for your specific case.
Preventive Measures
Prevention is key when it comes to plantar fasciitis. Maintaining a healthy weight to minimize the stress on your plantar fascia, choosing supportive footwear, and avoiding high-impact activities can reduce your risk.
If you're an athlete, incorporating foot exercises into your routine can help keep your plantar fascia from becoming overstressed.
When to See a Doctor
If you're experiencing persistent heel pain that doesn't improve with rest, ice, and over-the-counter pain relievers, it's time to see a doctor.
Also, if the pain is severe, swelling occurs, or you can't bear weight on your heel, you should seek medical attention promptly.
Early intervention can prevent plantar fasciitis from becoming a chronic condition.
Alternative Therapies
Some people find relief from plantar fasciitis through alternative therapies such as acupuncture, massage therapy, or chiropractic adjustments.
While scientific evidence supporting these treatments is limited, they may provide complementary benefits alongside conventional treatments. Always consult with a healthcare professional before trying alternative therapies.
Summary
Plantar fasciitis is an inflammation of the plantar fascia that causes heel pain, which can be debilitating. Understanding the causes, symptoms, and various treatment options is crucial for managing and overcoming this condition. With proper care, most people can recover from plantar fasciitis and return to their regular activities without lasting pain.
FAQ Section
Q 1: What is plantar fasciitis?
A: Plantar fasciitis is a prevalent foot condition characterized by inflammation of the plantar fascia, a thick band of tissue that runs along the bottom of the foot, connecting the heel bone to the toes.
This condition typically manifests as sharp or stabbing heel pain, particularly with the first steps in the morning or after prolonged periods of rest. Plantar fasciitis pain often improves with activity but can worsen again after prolonged standing or walking.
It is one of the most common causes of heel pain, affecting millions of individuals worldwide, and can significantly impact daily activities and quality of life.
Q 2: What causes plantar fasciitis?
A: Plantar fasciitis can develop due to various factors, including overuse, biomechanical issues, and certain risk factors. Overuse or repetitive strain on the plantar fascia, such as from activities like running, walking, or standing for long periods, can lead to microscopic tears and inflammation of the tissue.
Biomechanical issues, such as flat feet, high arches, or abnormal foot mechanics, can also contribute to the development of plantar fasciitis by placing excessive stress on the plantar fascia.
Additionally, factors like obesity, tight calf muscles, wearing unsupportive footwear, and sudden increases in physical activity levels can increase the risk of developing plantar fasciitis.
Understanding the underlying causes of plantar fasciitis is essential for implementing effective treatment strategies and preventive measures to manage the condition and prevent a recurrence.
Q 3: How is plantar fasciitis diagnosed?
A: Plantar fasciitis is typically diagnosed based on a thorough medical history, physical examination, and imaging studies, if necessary. During the physical examination, the healthcare provider will assess the affected foot for tenderness, swelling, and range of motion.
They may also perform specific maneuvers, such as the heel drop test or dorsiflexion test, to reproduce symptoms and confirm the diagnosis. In some cases, imaging studies such as X-rays or ultrasound may be ordered to rule out other possible causes of heel pain, such as fractures or heel spurs.
A comprehensive evaluation by a healthcare professional is essential for accurate diagnosis and the development of an appropriate treatment plan tailored to the individual's specific needs and lifestyle.